Renal replacement therapy.
ESRF, Hemodialysis and Peritoneal dialysis
Contents
- Renal replacement therapy
- Vascular access
- Complications
- Dialyser
- Dialysis prescription
- Medicines used in ESRD
- Peritoneal dialysis
_____________________________________
1-Renal replacement therapy - ESRD is irreversible functional and structural changes where life is incompatible without renal replacement therapy. Bloodletting started its journey to remove Toxins 300 yrs BC for chronic lifeterminating illness; Returning back washed, in 50's only. Innovative tummy wash came later in 60's. However, replacing body parts were attempted by Damian-Cosmas, the silverless one in 3rd century. Outcome was not known; however, they were decapitated for other reasons. Success achieved much later though, in last century.
Renal replacement therapy- a) Haemodialysis: HD, Online-HDF, SLED. b) Peritoneal dialysis: CAPD, CCPD, TPD, IPD. c) Transplant.
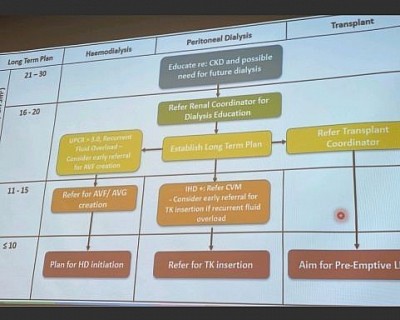
Initiation - Initiation is done in CKD patients without symptoms when glomerular filtration rate (eGFR) drops to 6 mL/min/1.73 m2 or until the onset of clinical indications like uremia, fluid overload, and refractory hyperkalemia or acidemia. Close monitoring should begin when eGFR reaches 15 mL/min/1.73 m2.
_____________________________________
2. Vascular Access for haemodialysis -
Permanent: a) AV Fistulla. b) AV Graft (PerchloroTetraFluroEthyline -PTFE, also known as Terumo graft, according to the discovering surgeon's name).
Temporary:
- Non-tunnelled Jugular (2- 6 weeks) or Femoral venous catheter (5-7 days). (Subclavian veins are not used because of high incidences of stenosis and thrombosis of centrsl vein).
- Tunnelled catheter (6 months to many years: to change yearly).
- HeRO graft (Hemodialysis Regular or Reliable Outflow graft): Single lumen tunneled IJ catheter (silicon rubber), tip at right atrium, other end connected by titanium with a PTFE graft, tunneled under the arm skin (for cannulation for dialysis), and connected to brachial artery. Used across Central vein stenosis.
_____________________________________
3. Complications
- Bleeding is a complication but uncommon.
- Other AVF complications are aneurysm formation, for which vascular surgeon ligate the vessel;
- AVF, AVG stenosis for which angioplasty also called fistuloplasty, are done;
- AVF, AVG thrombosis (includes HeRO graft, rt atrial clot formation and pulmonary embolisation) for which thromboplasty/thrombectomy are done.
- Other complication is steal syndrome resulting in distal ischaemia; here ligation of AVF is required.
- Catheter related bacterial infection. Less common with tunneled catheter and HeRO graft.
- Thrombosis is precipitated by low blood pressure, dehydration and hypercoagulable state. You need to increase DW, reduce erythropoietin, optimize Blood Pressure, look for thrombophilia test.
You may need to add Aspirin, long term with short or longterm Clopidogrel [DAPT], sometime you may need Warfarin (INR 2-2.5) or antithrombin (Argatroban).
_____________________________________
4. Dialysers technicalities
Dialysers, Toxins, Types of Dialyser, Dialyser membranes characteristics, Dialyser reuse:
Dialysers
Cylinders containing capillary tubes approximately 20 - 30 centimeters long with as many as 10,000 - 20,000 are clustered. The capillaries are made of Cellulose, nitro Cellulose, cupraphene, Polysulfone, polyacrylonitrate tube with exceptional filtering and hemocompatibility characteristics. The diameter of about 200 microm when wet. The membrane is about 20-45 micro thick, Pores in the capillaries filter metabolic toxins and excess water from the blood and flush them out of the body with dialysis fluid. Blood cells and vital proteins remain in the blood. These Semipermeable membrane let's the Diffusion of solute and Toxin from blood to counter-currently flowing Dialysate, happen (physical principle is Brownian movement of particles).
Toxins
Small molecules <500 Dalton, urea (60D), creatinine (113D), phosphate (134D). Middle molecules (MM 500-15000D), vitamin B12 (1355D), vancomycin (1448D), insulin (5200D), endotoxin fragments (1000-15000D), Parathromone (9425D), β2-microgobulin (11818). Large molecules > 15000D, myoglobin (17000), Retinol-Binding Protein (RBP) (21000D), EPO (34000D), albumin (66000D), Transferrin (9000D).
Types of dialyser
Low Flux (LF), high flux (HF), high efficiency (HE).
Natural Cellulose based and cupraphene membrane, Bio-incompatible (BI)
Synthetic polysulphone, polyacrylonitrate, biocpmpatible (BC).
Characteristics:
High-efficiency & Highflux( dialyser & hemofilter):
- High-efficiency: Numerous pores, thin membrane, and high surface area allowing high small molecule (urea) clearance. High efficiency hemofilter urea clearance (KoA) > 800-1000 mL/min.
- Dialyser urea clearance rate (KoA) is usually >210 mL/min.
- Ultrafiltration co-efficient (Kuf): Kuf is determined by Clearance of middle molecular weight molecules (β2 microglobulin).
- Highflux (Kuf) : Larger pores allowing better middle molecule (β2 microglobulin) clearance.
- Clearance of middle molecules (β2 microglobulin ) is high (>20ml/min).
- High UF means UF rate:10-20ml/hr/mmHg (Transmembrane pressure -TMP)
- Normal dialyser β2 microglobulin Clearance<10 ml/min.
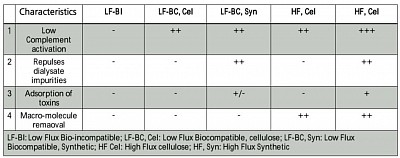
- Above table summarises the membrane characteristics.
Dialyser reuse
Two types:
- Manual cleaning with formalin and reuse for the same patient, max 6 times. The dialyser and the tubings were kept filed with formalin, labeled for respective patients.
- Renalin wash using automated machine, used Max 14 times. Fiber bundle volume min 80% to remain. After that discard. Now most dialysis centres use single use dialyser.
_____________________________________
5. DIALYSIS PRESCRIPTION
Dialysis blood flow rate is between (Qb) 200-400 ml/min. And dialysis fluid flow rate (Qd) counter-current to the blood flows in the dialyser cylinder is 2x blood flow. That mean 500 - 800 ml/min.
Normal AVF/AVG blood flow rate (Qa) is 800 - 1000 ml/min, for adequate dialysis.
Duration of dialysis (T) is usually 4 hours. Frequency 3 times per week.
When AVF/AVG flow rate (as measured by the nurses with flow meter machine) drops to less than 400 ml, interventional radiologist dilates it by angioplasty balloon.
Dialyser adequecy
Qb, Qd and time (T), along with dialyser clearance (K) & urea distribution volume (V), detetmine Dialysis adequacy (Kt/V). For details open the 'HD presentation for nurse' in this link.
Prescription for Dialysis:
- HD: Qb 200-400 ml/min, Qd 2xQb, T depending on KT/V to be delivered, UF 3-5% of pre HD weight. Heparin: 500-2000 unit Ist hour, 1/2 of initial dose hourly ranging from very tight to normal fraction. Alternatively, IV Fraxiparin 30-60 unit/Kg one dose.
- HDF: as above, but dialysate is reprocessed on-line running through additional two filters to make it infusible. 18-20% of this Dialysate runs as replacement fluid. Rest is used as Dialysate.
- SLED: Qb and Qd are reduced to 150 & 300 ml/ min respectively. SLED-F is same as HDF with SLED Qb and Qd.
- Isolated UF: Dialysate is bypassed.
- Modelled dialysis to avoid Intradialytic hypotension: a- UF Model- Ultrafiltration is done during initial period , b- Sodium model- Dialysate sodium concentration gradient is done from 150 to 135 mmol/L during the 4 hours dialysis. You can use high calcium Dialysate or iv albumin to avoid IDH.
Dialysate is a mixture of Dialysate concentrate and processed water in 1:40 ratio. Concentrate is mixture Na, CL, K, Ca, Mg, and glucose with Solution B containg bicarbonate. Final concentration (mmol/L): Na 140, K 2, Ca 1.5, Mg 0.5, Cl 111, Acetate 4, Bicarbonate 31, Glu 10.
_____________________________________
6. Medicines used in ESRD
In addition to the specific drugs for primary treatment of DM, hypertension, and other etiological factors, the following medicines are used:
- Anemia (target Hb 10-12g/dl) - a) Erythropoietin: 60-200 u/kg/week. b) Iron supplements (po/iv, target TS >25%).
- New medicine for Anaemia in ESRD: Roxadustat is a first-in-class orally administered inhibitor of
hypoxia-inducible factor (HIF) prolylhydroxylase that corrects anemia by a
mechanism of action that is different from that of erythropoiesis-stimulating
agents (ESAs). As a HIF-PH inhibitor, roxadustat activates a response that
occurs naturally when the body responds to reduced oxygen levels in the blood.
The response activated by roxadustat involves the regulation of multiple,
complementary processes to promote erythropoiesis and increase the blood’s
oxygen-carrying capacity. 20,50,100 mg 3 times a week in place of EPO, recently approved in Japan.
- Nutrition supplements: because of the dietary restrictions - a) Mineral and vitamin supplements. b) Protein - 1.2 g/kg in HD, 1.5 g/kg in PD. c) Ascorbic acid - <100 mg daily. d) Zinc sulfate - 50 mg daily (in deconditioned state). e) Water - 500ml/sqm in anuric state.
- Phosphate binders - CaCO3 (40% calcium), Calcium acetate (25% calcium), Lanthanum CO3, Sevelamer.
- PTH suppressant (target iPTH<25%) - Alfacalcidol or calctriol (contraindicated in Ca>2.4/PO4>2.4).
- Paracalcitriol - tertiary hyperparathyroidism.
- Calcimimetic (cinacalcet) - in tertiary hyperparathyroidism.
- Aspirin and clopidogrel - dialysis vascular access post thrombosis.
- H2 receptor blockers or PPI - uraemic dyspepsia.
- Anti itch medicines - Hydroxyzine tablets 10-25 mg and moisturizing urea are cream (10%) are used.
- ACEI or ARB - ESRD kidney is an endocrine organ, as such RAAS is active, that causes vicious increase in cardiovascular morbidity and mortality. ACEI or ARB are important drugs for ESRD.
- Furosemide - in case of residual renal function (RRF, urine output more than 100 ml/day), Furosemide can help maintain negative fluid balance reducing congestive states.
_____________________________________
7. Peritoneal dialysis
- For a synopsis of PD go to this link (Abridged from, Peritoneal Dialysis, Text Book of Nephrology, Brenner & Recter).
- For knowledge of advanced PD go to the link.
- For guidelines and landmark trial go to the links.
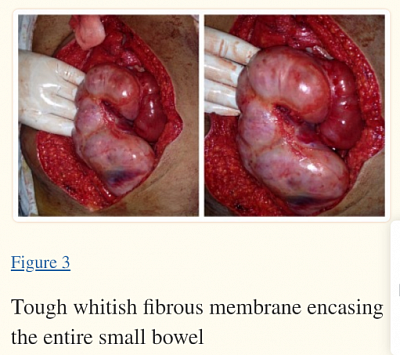
4. Some facts about EPS: it is progressive and life ending. Basic pathology is inflammation. It is precipitated by long duration of PD, use of high concentration of glucose solution, recurrent peritonitis and hemoperitoneum. Best strategy is the preventive strategy.
Follow the points to note:
- Early detection- first sign is hemoperitoneum. Change to HD once hemoperitoneum.
- Avoid higher glucose solutions.
- Prevent recurrent peritonitis.
- Use antifibrotic- ARB, ACEI, MRA. Questionable value of Tamoxifen.
- Once confirmed, patients die of malnutrition within 2 years.
- Stop PD after 7 years of initiation irrespective of events, and change to HD.