Acute Kidney Injury and Acute Kidney Disease
AKI & AKD
- Gonlomerular function assessment
- Tubular function assessment
- Urinary proteomics
- Segmental biomarkers
- Renal biopsy
6. Management and precautions for AKD
- Drug dosing in AKD
- Monitoring
- Non-drug management, renalfailureadvice.com
__________________________________
__________________________________
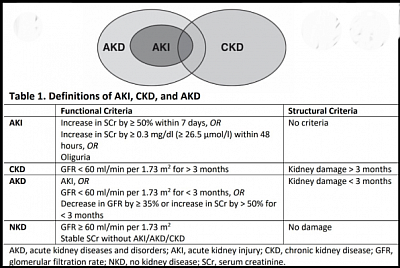
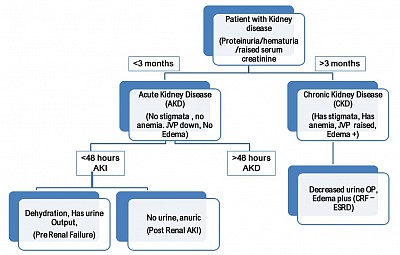
AKD, AKI & CKD
Based on Duration of kidney disease:
- AKI - Increase in serum creatinine or drop in urine output: in 24 Hours <7 days.
- AKD - (1) Any renal disease, with or without reduced eGFR or raised SCr (beyond laboratory reference limits), or urological disease (renal hypertension inclusive), or (2) continuation of AKI beyond 7 days at any AKIN or KDIGO stage (including RIFLE any category extending beyond 7 days) lasting not more then 90 days boundry <91 days.
- CKD - any damn kidney trouble >90 days.
_____________________________________
A dicotomous picture of Kidney diseases
_____________________________________
Section A: AKI
- What AKI does
- How AKI happens
- AKI classification
- What will you do
- Management
- Clinical types of AKI
- Pathophysiology and Morphological changes
- CRRT in AKI
- Fluid resuscitaion
- Further reading: ppx, trials, guideline. CRRT
_____________________________________
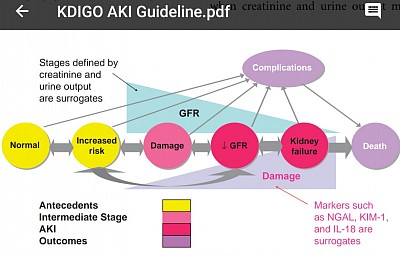
A1. AKI: What AKI does?
Progressive glomerular and Tubular damage as AKI progresses - explained in the figure below:
_____________________________________
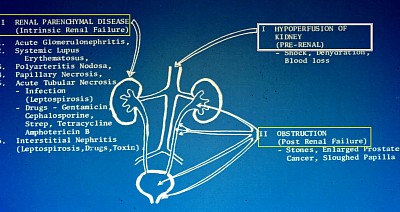
A2. HOW AKI happens?
Always remember the classic causes:
- Hypotension, dehydration, shock.
- Uncontrolled hypertension.
- Sepsis.
- Medications: NSAID, Nephrotoxic drugs, ARB, ACEI, MRA, etc.
- Exotoxins: Aristolachic acid (micro toxin from fungal growth on dried medicinal herbs (TCM causing AAN), phallotoxin from Amanita Phalloid in stale food etc.
- Obstruction: Urinary tract obstruction, renal artery and renal vein thrombosis.
- Endotoxins - rhabdomyolysis, tumor lysis, cholesterol emboli syndrome.
- MAHA states: HUS, TTP, TMA and DICS.
- Hepatorenal, Cardiorenal syndrome, obstetric complications.
_____________________________________
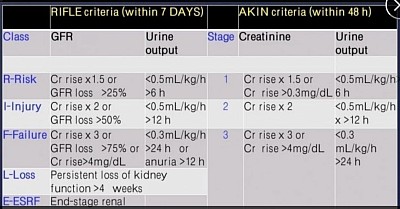
A3. Classification of AKI
- AKIN-1 & AKIN-2 need non-RRT management.
- AKIN-3 needs RRT support.
- When RRT exceeds 4 weeks, that is renal loss (L of RIFLE).
- When RRT exceeds 3 month, that is ESRD (E of RIFLE).
Available classifications for AKI
_____________________________________
A4. AKI: What will you do?
- having identified a patient with AKI?
- Look at the above obvious causes in history and physical examination.
- Is there obstruction? Do US KUB, confirm hydronephrosis. Do urinary catheterisation or percutaneous nephrostomy as appropriate.
- Any dehydration / hypotension? CVP line is preferred (CVP = 10-12 cm of water).
- Do fluid resuscitation with isotonic bicarbonate solution if there is metabolic acidosis.
- Treat Sepsis. Suspend NSAID/ ACEI-ARB/ MRA / Nephrotoxic drugs if in use.
- Check for rhabdomyolysis - look for CK-Aldolase.
- Check for acute glomerulonephritis - look for haematuria and proteinuria.
_____________________________________
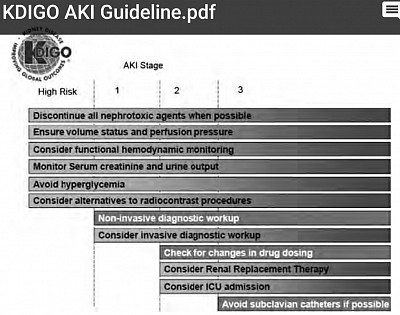
A5. AKI: Management of AKI
Manage accordingly:
- Acidosis, electrolyte anomalies and fluid balance.
- You may need to do renal biopsy.
- You may need RRT/ CRRT support allowing renal recovery.
- Follow KDIGO steps as shown in the figure.
_____________________________________
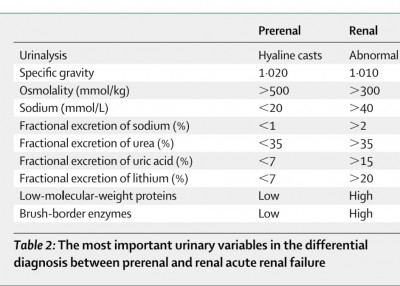
A6. AKI: Clinical types of AKI
After you have done the necessary resuscitation for AKI acutely, determine the clinical types of AKI as follows:
- Pre-renal AKI: in ischaemic AKI due to hypovolaemia or hypotension, prompt fluid resuscitation and blood pressure recovery, can prevent acute tubular necrosis (ATN). This state is known as Pre-renal AKI.
- Acute Tubular NECROSIS (ATN): ATN is of two types: ischaemic and Nephrotoxic.
Ischaemic - Prolonged ischaemia (24 - 48 hours, due to delayed fluid resuscitation and blood pressure recovery in cases of dehydration and shock) leads to necrosis of Tubular epithelial cells along with basement membrane (BM). This may lead to delayed recovery from AKI. This can also happen in renal artery stenosis, with use of ACEI, ARB, MRA and prostaglandin inhibitors.
Nephrotoxic - nephrotoxins cause epithelial cell necrosis leaving intact BM, thus recovery from ATN is faster.
- Post renal: (a) urinary tract obstruction, (b) renal vein thrombosis.
Established ATN needs supportive measures. Unrecovered cases of ATN progress to prolonged renal failure requiring dialysis.
Clinically it is necessary to differentiate prerenal AKI from ATN. Urinalysis as shown above can be used for this. FENa and FEUrea are definitive indicators of ATN.
_____________________________________
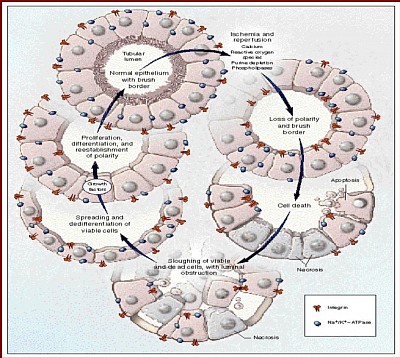
A7. AKI: Pathophysiology
- Morphological changes and inflammation:
Recovery occurs through Oliguric phase to Diuretic phase to Recovery phase. This is shown in the following figure:
Sepsis results in the release of damage- (DAMPs) and pathogen-associated molecular patterns (PAMPs), which are filtered at the glomeruli. These can lead to microcirculatory dysfunction,
increased oxidative stress, expression of tumor necrosis factor (TNF) receptors in the S2 segment tubular cells cell cycle arrest, namely tissue inhibitor of metalloproteinase 2 (TIMP-2)
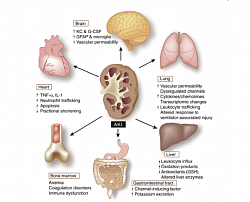
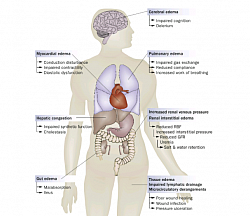
Acute kidney injury (AKI)-induced distant organ effects, including microvascular inflammation and coagulation, cell apoptosis, transporter activity, oxidative stress, and transcriptional responses.
Pathologic sequelae of fluid overload in organ systems. Abbreviations: GFR, glomerular filtration rate; RBF, renal blood flow.
Auto recovery of AKI in course of time
_______________________________
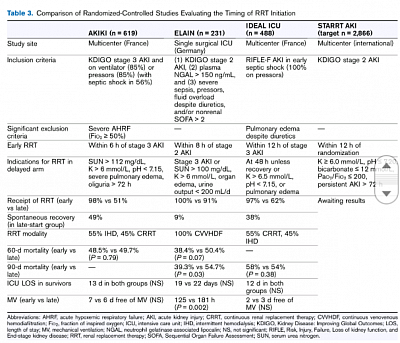
A8. AKI: IRRT / CRRT (IKRT/CKRT) in AKI
When AKI reaches stage 3 (KDIGO3) it may require dialysis (IRRT or CRRT) support.
IRRT: Haemodialysis and peritoneal dialysis can be used.
CRRT: However, in hemodynamically unstable patients continuous renal replacement therapy (CRRT) is indicated.
Please click on the next page for more information about CRRT.
A9. AKI: Fluid resuscitation
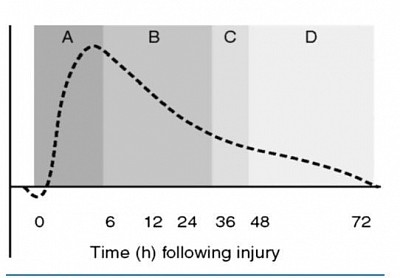
- Fluid resuscitation strategies in AKI correspond to the phases of critical illness and the immune response to sepsis or another injury.
- Phase A (0-6 hours): initial aggressive volume resuscitation (eg, 30 mL/kg of intravenous crystalloid), also known as the EBB phase of critical illness.
- Phase B (6-36 hours): decelerating fluid resuscitation; fluid is often still required to compensate for extravascular sequestration, but fluids should only be provided as needed to maintain organ perfusion in a targeted manner, with frequent reassessment of fluid responsiveness.
- Phase C (36-48 hours): equilibrium phase; fluid administration is stopped.
- Phase D (beyond 48 hours): mobilization, deresuscitation, or flow phase; fluids are withheld to allow for spontaneous diuresis or, in those who fail to autodiurese, pharmacologic diuresis or ultrafiltration can be provided to achieve euvolemia. The time of transition-phases may vary and multiple insults can substantially disrupt this sequence.
________________________________
________________________________
Section B
Contents:
AKD Continuation of AKI beyond 7 days until 90 days
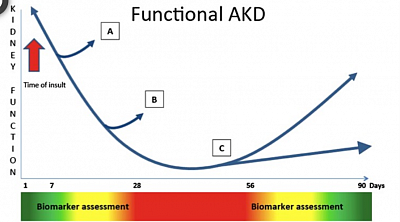
B1. AKD, initiation, pathogenesis and outcome:
- Initiation and progression of AKD, that followed AKI: [Fig: A]
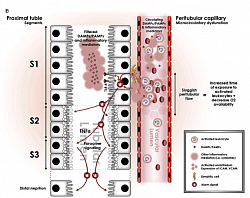
- Pathophysiology of AKD that follows AKI: [Fig: B]
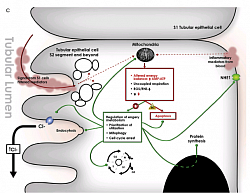
- Prognosis and Outcomes of AKD that follows AKI: [Fig C]
B2. AKD courses
- Deteriorating phase
- AKD Maintaining phase
- AKD Recovery phase
B3. Assessment of AKD.
- Glomerular function assessment
- Tubular functions assessment
- Urinary proteomics in AKD
- Segmental biomarkers
- Renal biopsy in AKD
B4. Management and precautions for AKD
- Drug dosing in AKD
- Monitoring of AKD
- Non-drug management of AKD: renalfailureadvice.com
________________________________
Section B: Acute Kidney Disease
Acute Kidney Injury progressing to Acute Kidney Disease, or De-novo kidney diease of less than 91 days. duration.
__________________________________
B1. AKD, initiation, pathogenesis and outcome described in Figure A, B, & C.
[Fig: A] Initiation and course of Acute Kidney Disease.
[Fig: B] Pathogenesis of Acute Kidney Disease.
[Fig: C] Prognosis and Outcome of AKD, in a 40 months prospective follow-up study using urinary proteomics in AKI at the onset. (Su, Woo, et al)
[Fig:A] After Acute Kidney Injury, the kidney has the ability to repair itself. With mild injury this repair can result in the return to a structural and functional state that is indistinguishable from normal. However, when the injury is more severe or is superimposed on baseline kidney abnormalities, the repair process can lead to fibrosis, which can facilitate progression to chronic kidney disease. Epidemiological studies now show that patients who have had AKI, have a marked increase in their risk for the development of end-stage renal disease.
[Fig:B] Recent data have redefined the role of the surviving epithelial cells in fibrosis and attribute myofibroblast expansion to perivascular and interstitial fibroblasts. After severe injury, the proximal tubule cellular response is impaired with its proliferative response altered due to cell cycle arrest at the G2/M phase of the cell cycle, resulting in generation of profibrotic factors including cytokines, growth factors and matrix proteins. Li Yang, Controversies in acute kidney injury. 2011;174:145-155
[Fig:C] Pathophysiologic factors for progression of AKI to AKD and subsequently to CKD/ESRD was studied, in a 40 months follow up study by urinary proteomics with SDSPAGE analysis of ICU admitted AKI cases, at the onset. AKI associated with glomerular proteinuria (mid and high molecular weight protein) had higher progression to AKD & CKD, than AKI with low molecular tubular proteinuria (P<0.5). This indicated, AKI associated with glomerlo-tubular injury has more progression than AKI with tubular injury alone. (Su, Woo et al, ref: Home & Study page, Section A\2 AKI\ AKI prospective study).
B2. Course of AKD as a continuation of AKI beyond 7 days
Course of AKD, that follows AKI, consists of three phases: as shown in the above cartoon.
- Deteriorating phase (green and yellow zone): when kidney function is actively worsening, (could improve as well, as shown in A direction).
- Maintenance phase (red zone): when the injury has ended but kidney function has yet to recover, (improvement can happen as shown in B direction).
- Improvement phase (yellow and green zone): where renal function begins to recover, ideally towards the preinjury baseline, (improvement can happen, or can progress to CKD as shown in the arrows).
_____________________________
B3. Assessment of AKD
- Glomerular function test by radio-isotope renogram or Inulin clearance or Cystatin-C clearance.
- Tubular function test by FEUrea, FENa
- Urinary proteomics
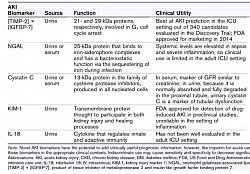
- Urinary Biomarkers in AKD
Nephron segment specific biomarker:
Glomerulus
Albumin
Cystatin-C
Proximal tubules
Albumin
Clusterin
IGFBP7
KIM‐1
L‐FABP
NAG
NGAL
Osteropontin
TIMP‐2
Loop of Henle
Osteopontin
Distal tubules
Clusterin
NAG
NGAL
OsteopontinA
Collecting duct
Calbindin D28
[Adreviations: IGFBP7, insulin‐like growth factor‐binding protein 7; KIM‐1, Kidney injury molecule‐1; L‐FABP, Liver‐type fatty acid binding protein; NAG, N‐acetyl‐β‐D‐glucosaminidase; NGAL, neutrophil gelatinase‐associated lipocalin; TIMP‐2, Tissue inhibitor of metalloproteinase 2]
- Renal biopsy
Renal biopsy would distinguish GN, IN, ATN, DN, Secondary FSGS, IF, TA, CNI toxicity Allergic IN, CPN and normal kidney.
_____________________________
B4. Drug management during different phases of acute kidney disease:
Drugs administration have to be eGFR (point 7) dependant.
Drugs handled by relevant nephron segments:
Glomerulus
- Doxorubicin
- Gold
- Penicillamine
Proximal tubule
- Amikacin
- Cisplatin
- Colistin
- Cyclosporine
- Gentamicin
- Hydroxyetheyl starch
- Tacrolimus
- Tobramycin
- Vancomycin
Loop of Henle
Analgesics (chronic)
Distal tubule
- Amphotericin B
- Cyclosporine
- Sulfadiazine
- Tacrolimus
Collecting tubule
- Ampotericin B
- Acyclovir
- Lithium (acute)
_____________________________
B5. Monitoring with fortnightly follow up.
(This can be done by APN at Polyclinic unless changes in medicines are required).
_____________________________
Strategies to halt AKD by lifestyle changes, protective and preventive strategies to stop AKD progression, changes in diet style, and kidney disease prevention education.
_____________________________

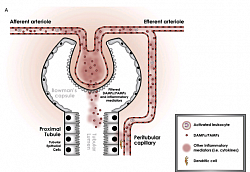
![[Fig:A] After Acute Kidney Injury, the kidney has the ability to repair itself. With mild injury this repair can result in the return to a structural and functional state that is indistinguishable from normal. However, when the injury is more severe or is superimposed on baseline kidney abnormalities, the repair process can lead to fibrosis, which can facilitate progression to chronic kidney disease. Epidemiological studies now show that patients who have had AKI, have a marked increase in their risk for the development of end-stage renal disease.](images/th/sd_5feddff0390e3.png?no_cache=1711930880)
![[Fig:B] Recent data have redefined the role of the surviving epithelial cells in fibrosis and attribute myofibroblast expansion to perivascular and interstitial fibroblasts. After severe injury, the proximal tubule cellular response is impaired with its proliferative response altered due to cell cycle arrest at the G2/M phase of the cell cycle, resulting in generation of profibrotic factors including cytokines, growth factors and matrix proteins. Li Yang, Controversies in acute kidney injury. 2011;174:145-155](images/th/sd_5fede0468b267.png?no_cache=1711930900)
![[Fig:C] Pathophysiologic factors for progression of AKI to AKD and subsequently to CKD/ESRD was studied, in a 40 months follow up study by urinary proteomics with SDSPAGE analysis of ICU admitted AKI cases, at the onset. AKI associated with glomerular proteinuria (mid and high molecular weight protein) had higher progression to AKD & CKD, than AKI with low molecular tubular proteinuria (P](images/th/sd_5fee26676b11a.png?no_cache=1711930919)